Mean corpuscular hemoglobin (MCH)
Bottom line: The MCH and MCHC are often reported side by side in a CBC panel. This causes confusion for those not familiar with the difference between the two parameters. The MCHC is helpful in classifying anemia. The MCH is not. The MCH, which tracks with the MCV and MCHC, adds little information to that imparted by the latter two parameters. Owing to the risk of confusion and the lack of useful information, consider ignoring the MCH altogether.
- What is the MCH?
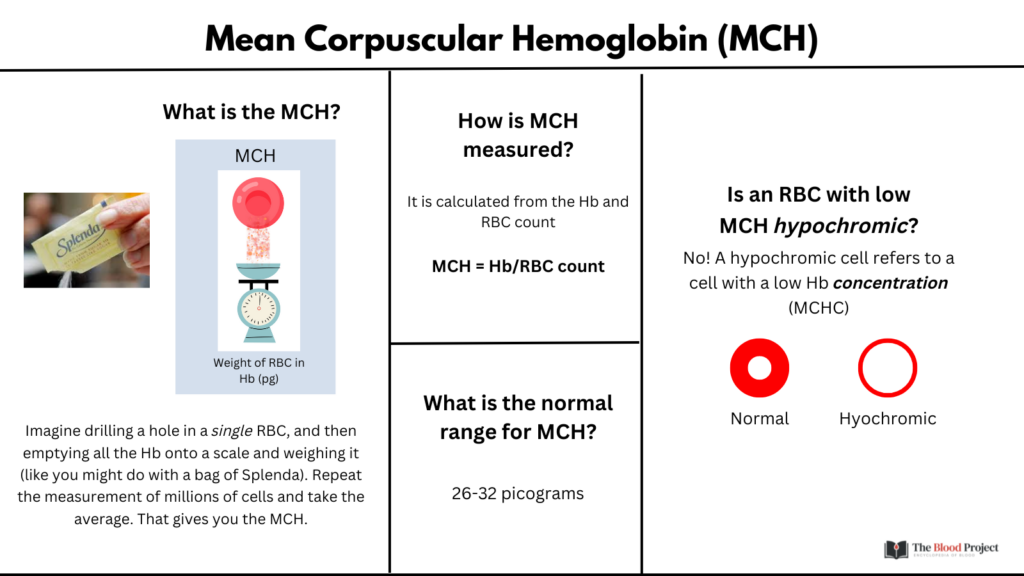
- The MCH refers to the average weight of hemoglobin (Hb) inside a single red blood cell (RBC).1
- Imagine drilling a hole in a single RBC, and then emptying all the Hb onto a scale and weighing it (like you might do with a bag of Splenda). Repeat the measurement in millions of cells and take the average. That gives you the MCH.
- How is MCH calculated?
- The MCH is not directly measured. Rather, it is calculated from the Hb and RBC count:
- MCH = Hb/RBC count
- The MCH is not directly measured. Rather, it is calculated from the Hb and RBC count:
- What is the normal range for MCH?
- 26-32 picograms or 10-12 grams.
- So how does the MCH differ from the MCHC?
- The mean corpuscular Hb concentration (MCHC) is the average weight in Hb per RBC volume.
- The MCH is not directly measured. Rather, it is calculated from the Hb and Hct:
- MCHC = Hb/Hct
- Note that while the MCH is a weight, the MCHC is a concentration.
- The MCH and MCHC are not necessarily concordant.
- For example, consider a teeny tiny spherocyte, a tenth of the size of a normal RBC. Its weight in Hb will be low, but its Hb concentration will be high (think about how spherocytes lack central pallor).
- Is an RBC with low MCH hypochromic?
- No! The term hypochromia refers to a cell with a low Hb concentration (i.e., a low MCHC)
- Any RBC, no matter how small or large in size, that has a reduction in Hb proportional to cell volume (think of an RBC with increased central pallor) is considered hypochromic.
- What’s more useful: the MCH or the MCHC?
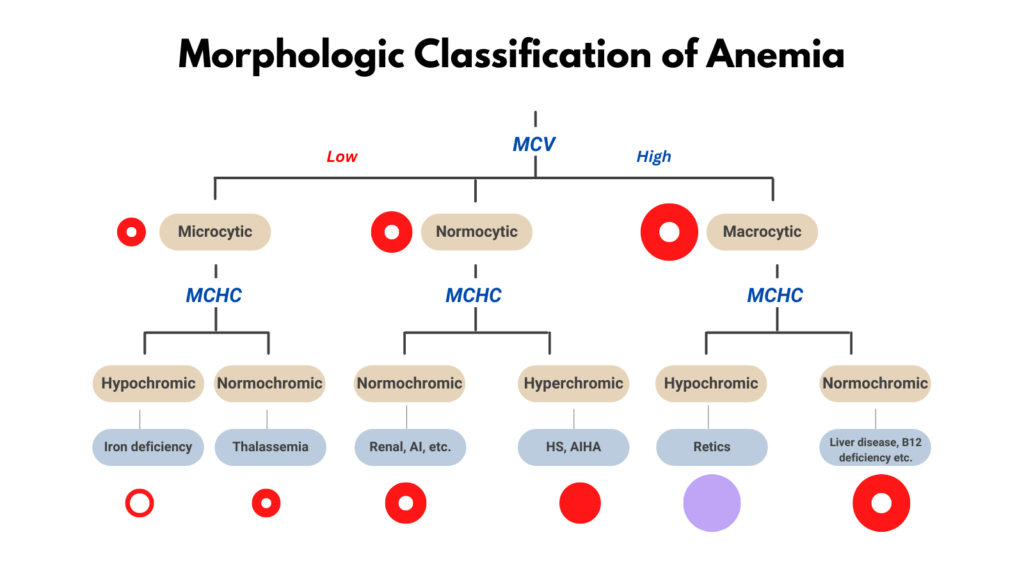
- The MCHC is much more helpful than the MCH in clinical practice.
- The MCHC, but not the MCH, is part of the diagnostic algorithm for anemia (see graphic).
- So how is MCH helpful?
- It really isn’t that useful. What’s more, it often gets confused with the MCHC.
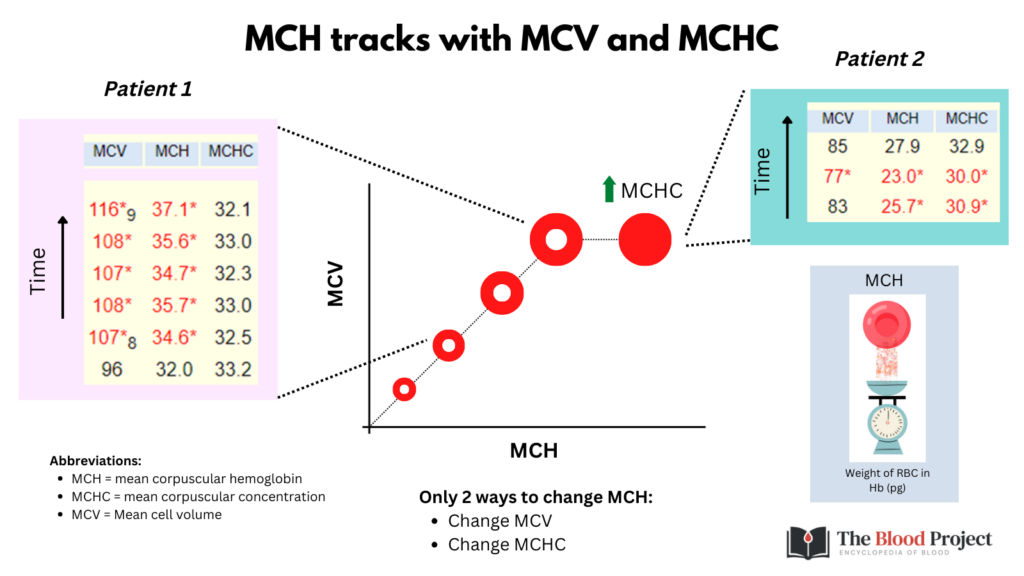
- The MCH is redundant: it tracks with the MCV and MCHC (MCH = MCV x MCHC).
- It has been argued that the MCH is a surrogate for the MCV. But if the MCV is available, who needs a surrogate (OK, in the rare case of an in vitro artifact – see below)?
- There are only 2 situations in which the MCH provides more information than the MCV or MCHC alone:
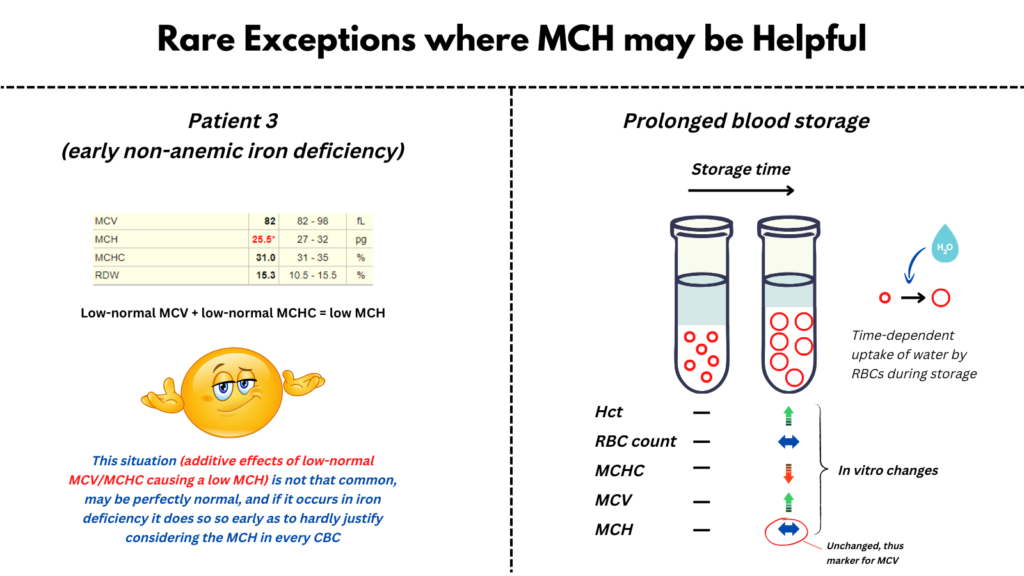
- Early iron deficiency: MCH = MCV x MCHC, and since both MCV and MCHC tend to decrease in iron deficiency, MCH is more sensitive than either MCV or MCHC. You can imagine a situation where the MCV and MCHC have decreased to the low-normal range in early iron deficiency (still impetrated as “normal”), resulting in a slight drop in MCH below the normal range. If your goal is to pick up as many cases of early non-anemic ID as possible, then have at it! Otherwise, make life easier and ignore the MCH.
- Artefactual changes in the MCV: The MCH is admittedly a useful surrogate for MCV in situations where the MCV is artifactually altered, for example with prolonged storage of blood as might occur when blood is shipped long distance or stored during space flight.
For quiz, click here.
