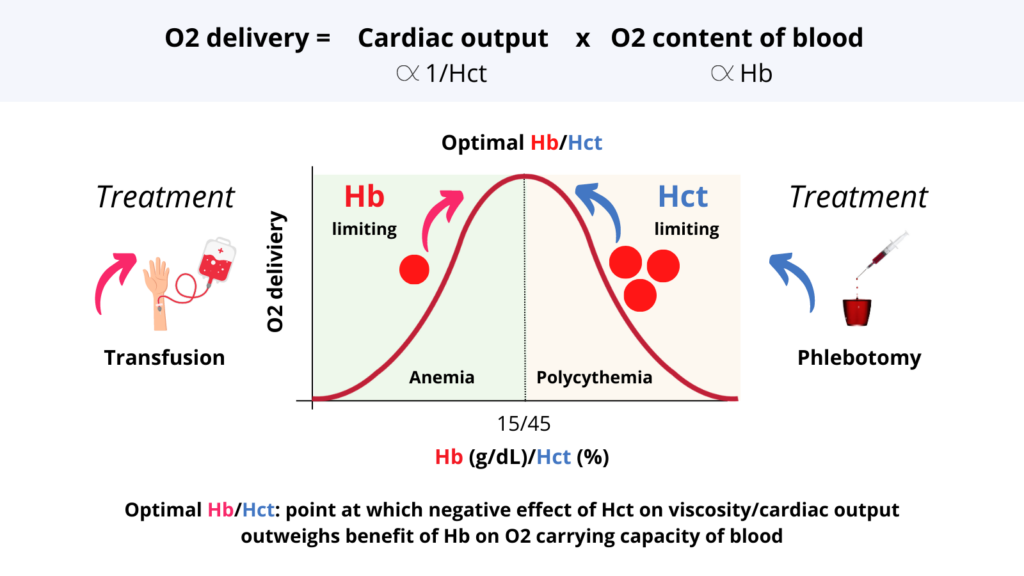
1. O2 delivery (DO2) = cardiac output (CO) x O2 content of blood.
2. O2 content of the blood correlates positively with Hb.
3. CO correlates negatively with Hct (through its effect on blood viscosity).
4. DO2 as function of Hb/Hct = bell-shape curve.
5. As Hb/Hct increases, so too does DO2 until the negative effect of Hct on DO2 offsets the positive effect of increased Hb on O2 content.
6. The peak of the curve is called the optimal Hb/Hct (about 15 g/dL and 45%, respectively) and is conserved across mammalian species.
7. Patients who live on ascending part of curve have anemia. The goal of treatment is to nudge them up the hill towards the summit, e.g. with Fe or B12 treatment, or transfusion.
8. The rare patient on the descending part of the curve has polycythemia. Here the goal is to pull them back up the hill towards the summit, e.g. with phlebotomy or myelosuppressive agents.
9. So, it makes sense to talk about Hb when referring to a patient with anemia, and the Hct when referring to one with polycythemia. And indeed, that is the approach taken by clinical practice guidelines: Hb trigger in anemia, Hct threshold for phlebotomy in polycythemia.
10. As for those who live at/near the peak of the mountain (most of us), it’s dealer’s choice whether to use Hb or Hct, but how ’bout thinking on the “positive” side and using Hb (after all the Hct is simply a necessary trade-off/cost for packaging Hb inside cells).
