Knowledge Check
Which of the following statement is/are true concerning the difference between a reticulocyte and a mature red blood cell:
True of false: reticulocytes can be seen on a Wright-Giemsa stained peripheral smear.
Which one of the following statements is correct?
Which one of the following statements is/are correct related to the life cycle of a reticulocyte?
True or false: reticulocytes in the peripheral blood are homogeneous in appearance.
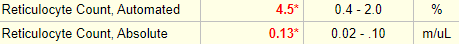
True or false: the absolute reticulocyte count provided autocorrects for the degree of anemia.
True or false: at steady state, approximately 1 to 2 percent of circulating RBCs are reticulocytes, corresponding to an absolute reticulocyte count of approximately 25,000 to 100,000/microL (0.25 to 1 x 1011/L).











In addition to correcting for anemia, another correction factor has been advocated by some. What is it?
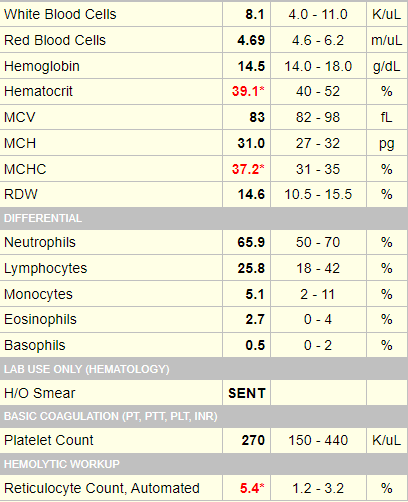
Click for AnswerTrue or false: the absolute reticulocyte count autocorrects for maturation time.
Correcting for the maturation time according to the degree of anemia assumes that there is an inverse correlation between the patient’s Hb and reticulocyte maturation time in the circulation. However this has never been definitively shown. Moreover, if there is such a correlation it probably applies only to cases in which there is active erythropoiesis (i.e., a healthy marrow is spitting out younger than normal reticulocytes). According to the reticucyte production index (RPI) formula, the reticulocyte percentage is “downgraded” in such situations. It is difficult to see how that is helpful when all we are trying to do is differentiate between a hypo- and hyperproliferative state.
Assuming the absolute reticulocyte count is all we really need, what is the threshold value for differentiating between a hypo- and hyperproliferative state











The patient has a normal Hb, so why do we even need to consider the reticulocyte count?
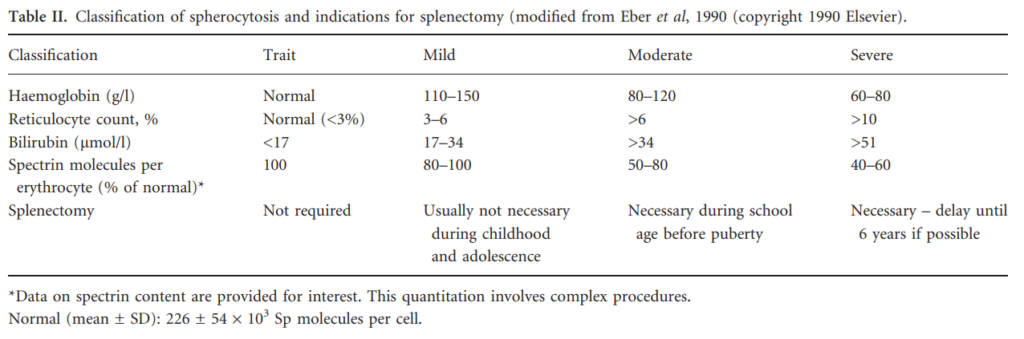
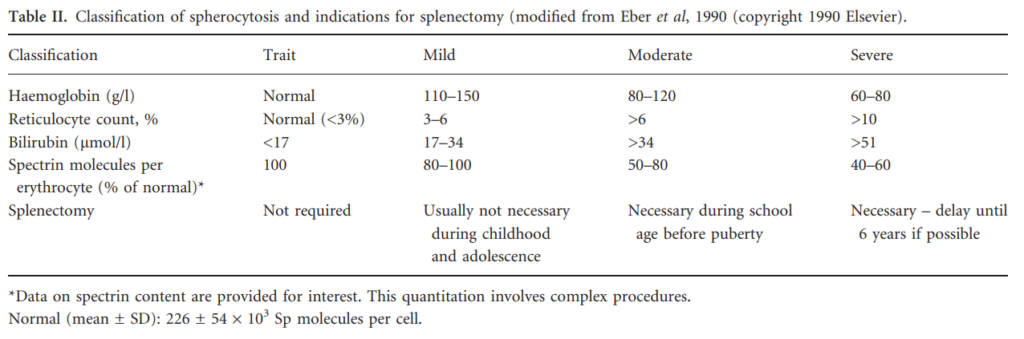
Click for AnswerThis was a case of hereditary spherocytosis. We have discussed the lack of utility in scoring degrees of reticulocytosis (over and above using the threshold number to determine whether an anemia is hypo- or hyperproliferative). However, there are exceptions, including the use of different degrees of reticulocyte (crude!) percentages to classify severity of hereditary spherocytosis:
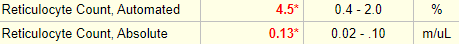
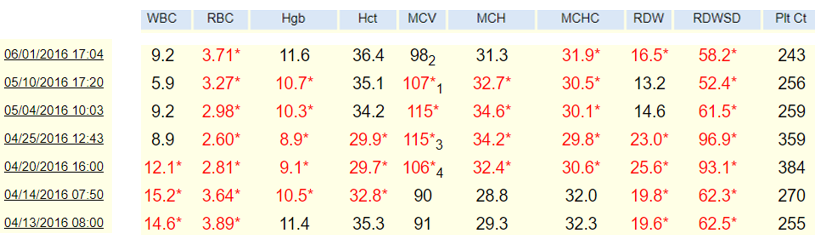
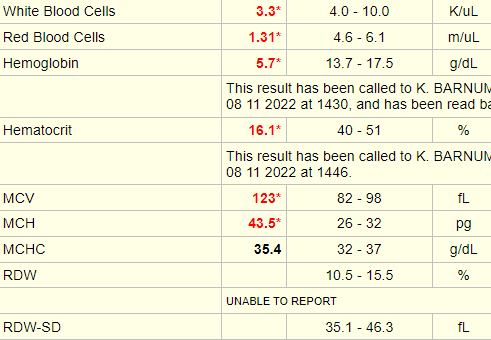
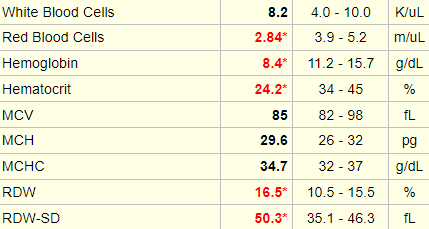
Does the following patient have anemia?
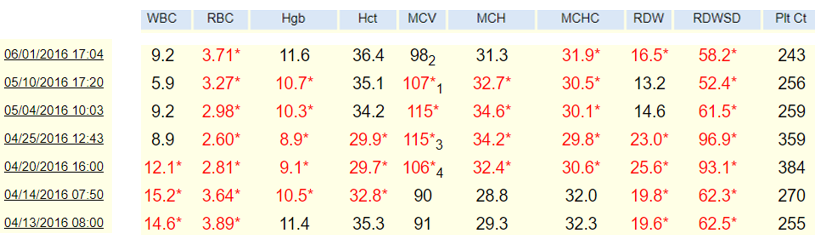
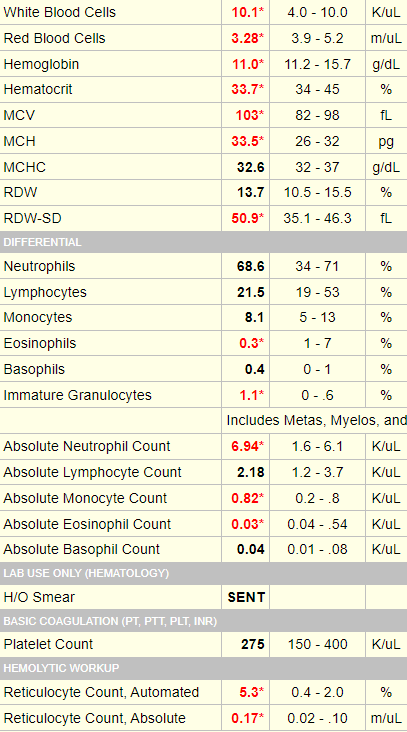
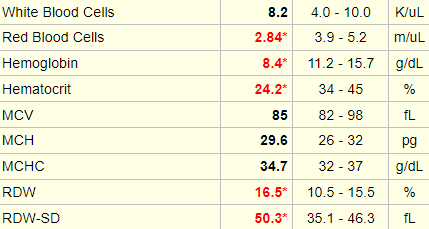
The following is the CBC from the last case.
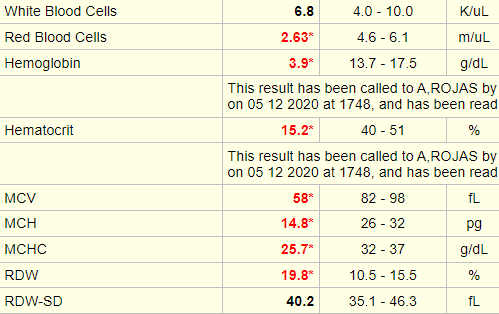
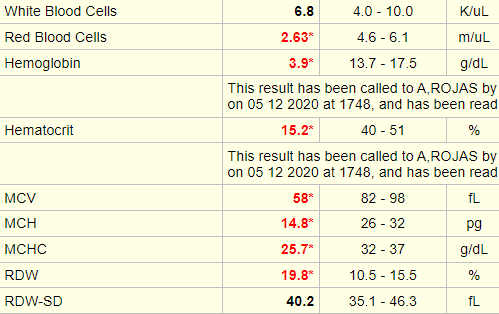
What is this patient’s corrected reticulocyte percentage (reticulocyte index)?
Answer on the next slide.
What is this patient’s corrected reticulocyte percentage (reticulocyte index)?
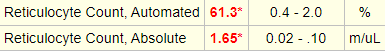
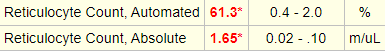
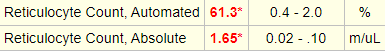
Answer on the next slide.
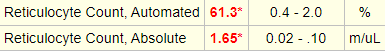
Red cell count = Absolute retic count/retic % = 1.65 x 1012/L/0.613 = 2.69 x 1012/L (normal 4.5-6.0 x 1012)
Reticulocyte index = Retic % x patient’s RBC count/normal RBC count = 61.3 x 2.69/5* = 33%
* Assumes normal RBC count of 5 x 1012
One of the most striking differences between pyruvate kinase deficiency (PKD) and most other hereditary hemolytic anemias is the dramatic post-splenectomy reticulocytosis that occurs in PKD, which usually increases 50% or more over pre-splenectomy counts. Reticulocytes have a much higher ATP requirement as compared with mature red cells but can rely on oxidative phosphorylation for energy. However, in the hypoxic splenic environment, PK deficient reticulocytes must rely on glycolysis, which does not meet the ATP needs, leading to hemolysis. In the absence of the spleen, reticulocyte survival increases. Haematologica. 2020;105(9):2229-2239.
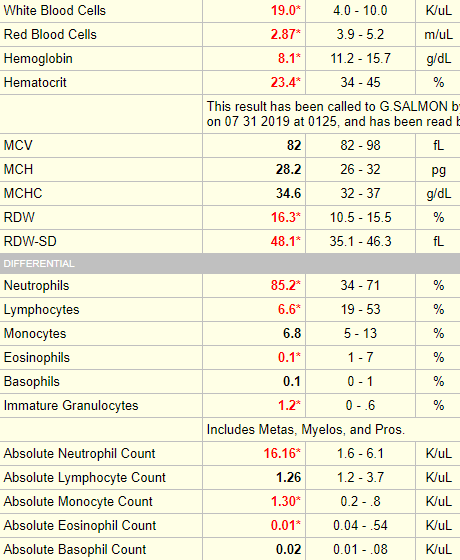
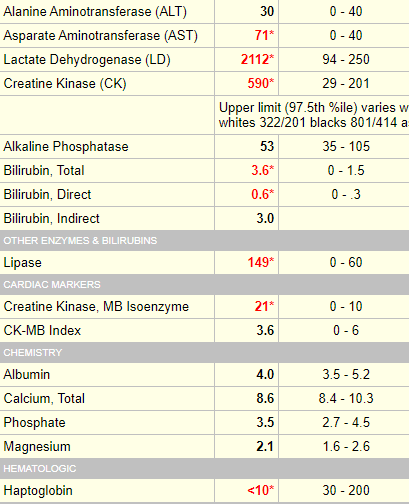
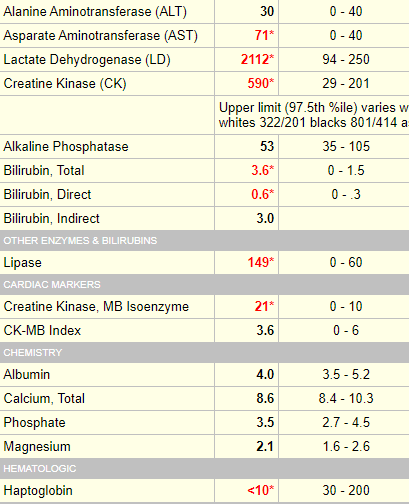
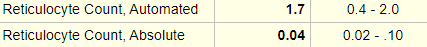
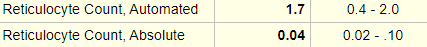
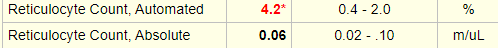
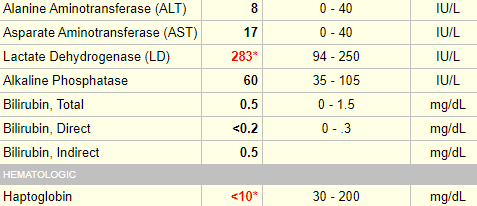
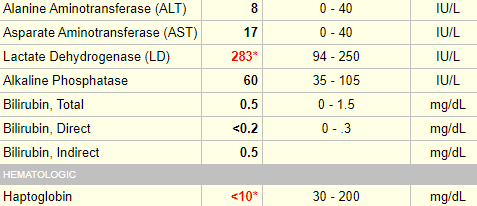
The following patient is hemolyzing (that is the reason for the elevated serum LDH and undetectable serum haptoglobin). A calculation of the RBC count from the reticulocyte percentage and absolute retic count demonstrates clear cut anemia. Is the patient’s reticulocyte response appropriate? After all it is 4.2%, which is higher than the normal range provided by the lab.
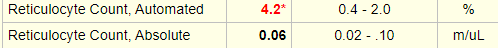
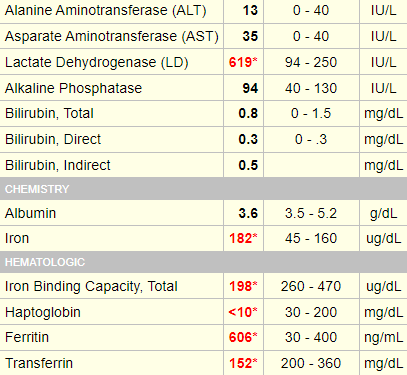
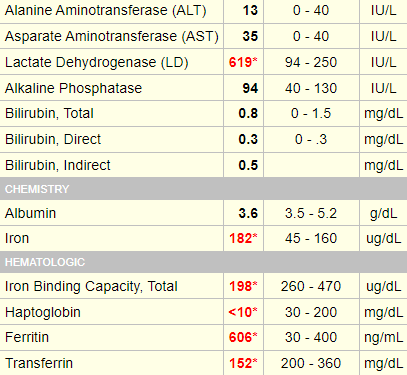











How do you explain an inappropriate retic response in the setting of hemolytic anemia?
Click for AnswerHere is the CBC from the previous case:
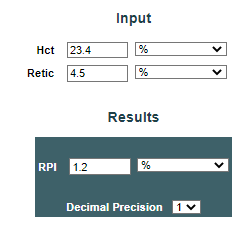
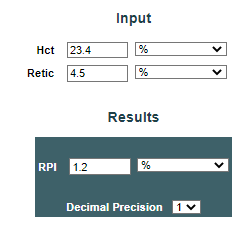
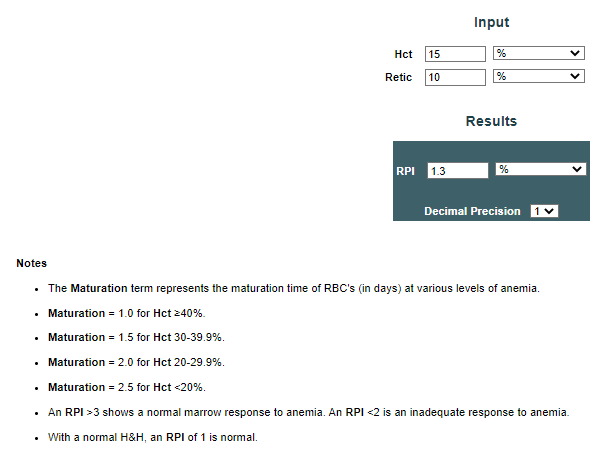
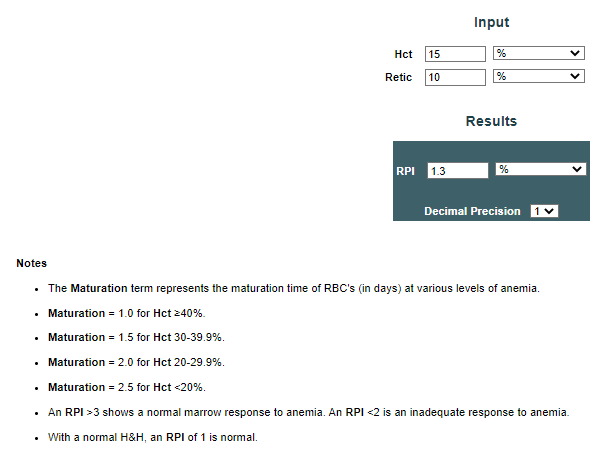
Let’s consider this whole business about adding a second correction factor to the reticulocyte index or absolute reticulocyte count (remember, both of the latter serve to correct for patient’s Hb/Hct) to correct for maturation time. The reticulocyte maturation index (or reticulocyte production index) corrects for both the Hb/Hct and for the maturation time (the latter, in turn, is derived from the Hb/Hct and is based on some limited previously published data). A calculator for the RPI can be found here.
| ARC | RPI | |
|---|---|---|
| Retic 3%; Hct 25; RBC 3.12 | 93.6 | 0.8 |
| Retic 4%; Hct 25; RBC 3.12 | 125 | 1.1 |
| Retic 5%; Hct 25; RBC 3.12 | 156 | 1.4 |
| Retic 3%; Hct 15; RBC 1.88 | 56 | 0.4 |
| Retic 4%; Hct 15; RBC 1.88 | 60 | 0.5 |
| Retic 5%; Hct 15; RBC 1.88 | 94 | 0.7 |
| Retic 8%; Hct 15; RBC 1.88 | 150 | 1.1 |
| Retic 10%; Hct 15; RBC 1.88 | 188 | 1.3 |
| Retic 20%; Hct 15; RBC 1.88 | 376 | 2.7 |
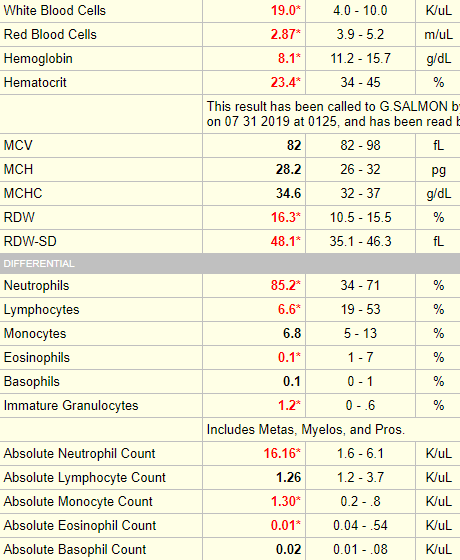
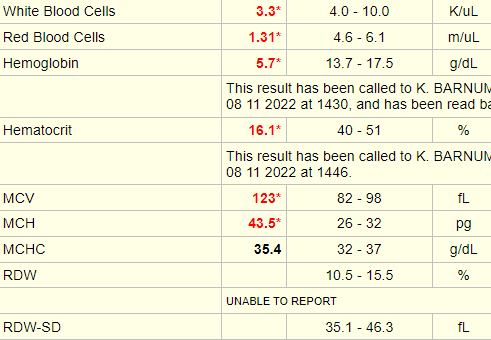
Now let’s look at some real cases. The case below is 67 year-old M with autoimmune hemolytic anemia. The complete blood count shows anemia, and the hemolytic indices (serum LDH and haptoglobin) are positive. Note that the absolute reticulocyte count of 0/17 x 1012/L or 170 x 109/L is more than enough to qualify for appropriate response (i.e. hyperproliferative anemia), whereas the reticulocyte maturation index (or reticulocyte production index) is below the threshold value of 3 for hyperproliferative anemia.
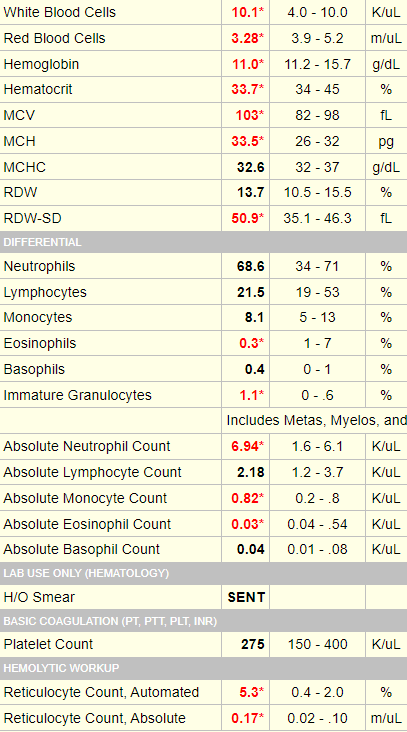
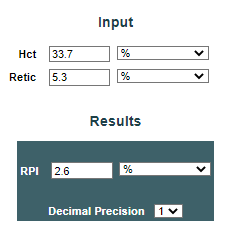
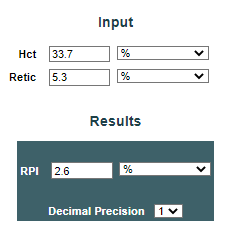
The following is another case of autoimmune hemolytic anemia. Again, the patient has anemia and positive hemolytic makers, and again, the absolute reticulocyte, and not the reticulocyte maturation index (or reticulocyte production index), correctly identifies the anemia as hyperproliferative.
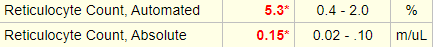
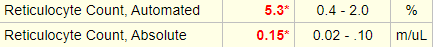
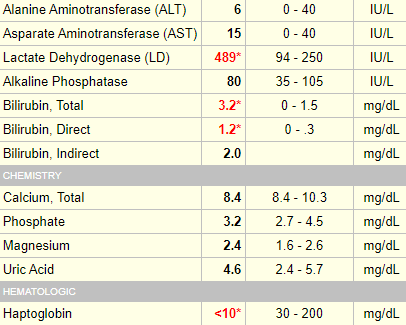
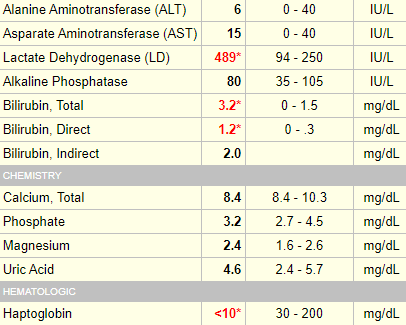
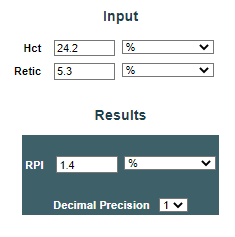
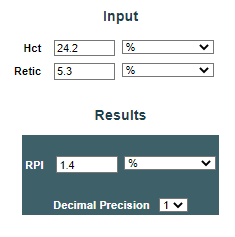
One more case, this time of thrombotic thrombocytopenia purpura. Again, the reticulocyte maturation index (or reticulocyte production index) fails us.